- Hemwellectomy Vs. Doppler-Guided Hemorrhoid Surgery: A Comparative Overview
Medical Advisory Board
Chief Medical Officer
Introduction
This article compares the Hemwellectomy procedure—a low-energy electrosurgical approach—to the Doppler-guided transanal dearterialization with mucopexy (“surgery”). Although both techniques aim to reduce hemorrhoidal blood flow, they differ markedly in their mechanisms of action, postprocedural pain profiles, and overall complication rates.
Surgical Technique and Mechanism
Doppler-Guided Transanal Dearterialization with Mucopexy
Doppler-guided surgery utilizes a transanal Doppler probe to identify the arterial supply to hemorrhoids. The identified arteries are ligated, thereby reducing or eliminating the afferent blood flow. In a subsequent step, the prolapsed tissue is plicated (mucopexy), repositioning it back into the rectal submucosa. Although initially intended to decrease postoperative pain, several studies indicate that pain remains a significant concern following this procedure (1).
Hemwellectomy
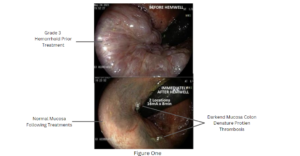
Hemwellectomy employs a two-pronged, rounded probe (serving as the cathode) that is applied directly at the base of the hemorrhoid or onto the hemorrhoidal tissue. The procedure administers a continuous, low-energy direct current (16 mA), similar in magnitude to that used in temporary transvenous pacemakers. This low-energy current induces sustained smooth muscle contraction, resulting in profound vasospasm closing off the hemorrhoid’s arterial supply. Unlike the doppler-guided technique, Hemwellectomy’s non-thermal mode of action spares the overlying mucosa, thereby mitigating postoperative pain and other complications. Veins, without a smooth muscle media, are also spared, allowing blood to leave the hemorrhoid which shrinks to the submucosa. (Fig 1)
Electrophysiological and Biochemical Effects
Both techniques aim to de-arterialize hemorrhoidal tissue, but they differ in their underlying mechanisms:
Vasospasm: Hemwellectomy’s continuous direct current produces sustained contraction of the smooth muscle in the arterial wall, leading to immediate and effective vasospasm. In contrast, doppler-guided ligation mechanically occludes the arteries. (fig 2)
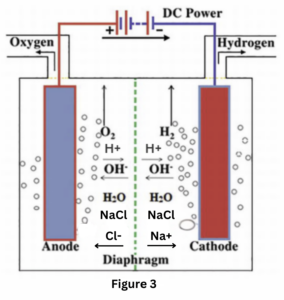
Electro-biochemical Reactions: The Hemwellectomy procedure harnesses a series of electro-biochemical events. As the low-voltage current is applied, electrolysis occurs in the electrolyte-rich serum, splitting water into H⁺ and OH⁻ ions. The generation of hydrogen gas at the cathode results in visible, soapy, hydrogen-filled bubbles that are a byproduct of saponification. This process not only confirms the local electro-biochemical reaction but also contributes to the dearterialization by altering the local pH and promoting thrombosis in the arterial vessels. (Fig 3)
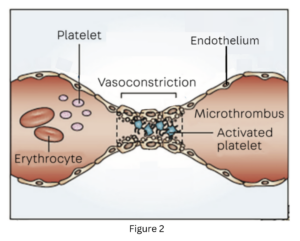
Platelet Activation and Thrombosis: The continuous current also directly affects endothelial cell membranes and activates platelets, contributing to the permanent ligation by thrombosis of the hemorrhoidal arterial supply. (fig 2)
Clinical Efficacy and Safety
Doppler-Guided Surgery
Clinical studies report that doppler-guided dearterialization with mucopexy offers similar efficacy to conventional hemorrhoidectomy in terms of symptom relief. However, postoperative pain remains a significant limitation, potentially offsetting its less invasive intent.
Hemwellectomy
In contrast, Hemwellectomy has demonstrated a success rate exceeding 90% with a single treatment. The procedure’s targeted mechanism results in effective dearterialization with minimal collateral tissue damage. Importantly, Hemwellectomy is associated with negligible postoperative pain, and serious complications have not been reported in over 100,000 procedures since FDA approval.
Conclusion
While both doppler-guided surgery and Hemwellectomy aim to reduce the arterial blood supply to hemorrhoids, the latter offers distinct advantages. Hemwellectomy achieves its effect through a unique electrosurgical mechanism that induces sustained vasospasm, targeted thrombosis, and electro-biochemical reactions without thermal injury. This results in highly effective treatment with a superior safety and tolerability profile, making it the procedure of choice for the full spectrum of hemorrhoidal disease.
References
- De Nardi, P., Capretti, G., Corsaro, A., & Staudacher, C. (2014). A prospective, randomized trial comparing doppler-guided transanal hemorrhoid dearterialization with mucopexy versus excision hemorrhoidectomy for grade III hemorrhoids. Diseases of the Colon and Rectum, 57(3), 348-353.
- LaPelusa, A., & Dave, H.D. (2023, May 1). Physiology, Hemostasis. StatPearls. Treasure Island, FL: StatPearls Publishing.
- Chen, W. (2005). Electroconformational denaturation of membrane proteins. Annals of the New York Academy of Sciences, 1066, 92-105.
- Hardy, E., Sakurai, Y., Sanjaya, N., Wolberg, A.S., & Lam, W. (2012). Effect of locally applied electricity on clot formation and hemostasis. Blood, 120(21), 2220.
- Sedlarik, K. et al. “Electro-thrombosis and alternative to embolization using particles.” Rofo, 1981.
- Sedlarik, K. et al. “Electrothrombosis as a treatment.” Z Exp Chir, 1981.
- Yada, Y. et al. “Submucosal Electrocoagulation of Prolapsed Hemorrhoids: A New Operative Approach.” Acta Med Okayama, 2010; 64(6): 359-365.
- Norman, D. “Direct Current Electrotherapy of Internal Hemorrhoids: An Effective, Safe and Painless Outpatient Approach.” Am J Gastroenterol, December 1988.
- Olatoke, S., Adeoti, M., Agodirin, O., Ajape, A., & Agbola, J. (2014). Direct current electrotherapy for internal hemorrhoids: experience in a tertiary health institution. Pan Afr Med J, 18, 145.
