- Hemwellectomy: A Novel Electrosurgical Approach for Hemorrhoidal Disease
Medical Advisory Board
Chief Medical Officer
Introduction
Hemwellectomy first performed in 2022, represents an innovative, FDA‐approved electrosurgical treatment for hemorrhoidal disease spanning grades I through IV. Unlike office-based therapies that are limited to lower grades, this procedure offers a comprehensive option for managing the full spectrum of hemorrhoidal pathology encountered in primary care, gastroenterology, and surgical practices. This review outlines the epidemiology and pathophysiology of hemorrhoidal disease, examines conventional treatment modalities and their associated complications, and then details the scientific principles, procedural technique, and clinical efficacy of Hemwellectomy.
Epidemiology and Clinical Presentation
Hemorrhoidal disease is the fourth most frequent gastrointestinal diagnosis in outpatient settings, accounting for approximately 3.3 million ambulatory care visits annually in the United States. An estimated 10 million individuals self-report hemorrhoids each year, with peak prevalence noted between 45 and 65 years of age. Demographic data indicates a higher incidence in Caucasian populations and among individuals of higher socioeconomic status. Although not associated with high mortality, the symptom burden—including rectal bleeding, prolapse, pain, and pruritus—can significantly impair quality of life.
Pathophysiology and Anatomical Considerations
Historically misinterpreted as simple varicosities, hemorrhoids are now understood as the pathological herniation of the anal cushion into the rectal lumen. The normal anal cushion is a highly vascularized, sinus-like structure supplied by terminal branches of the superior rectal artery, with drainage occurring via both the portal and systemic venous systems. In the setting of hemorrhoidal disease, these arterial branches exhibit increased diameter and flow, contributing to the development and progression of the condition. Concomitant venous dilatation further exacerbates symptomatology.
Conventional Treatments and Their Limitations
Initial management of hemorrhoidal disease typically involves conservative measures such as dietary modifications, topical therapies, and laxatives. When these fail, office-based procedures, most notably rubber band ligation, sclerotherapy, and infrared coagulation—are considered. These office-based procedures, although widely used, are approved only for grades I, II and some grade III hemorrhoids and are associated with complications including pain, bleeding, vaso-vagal reactions, allergic reactions, and, in rare instances, serious outcomes such as urinary retention, sepsis, and even death. Surgical hemorrhoidectomy remains the definitive treatment for refractory grade III and IV disease; however, it invariably produces sever postoperative pain, prolonged recovery (with return to work typically delayed three or more weeks), and other complications such as bleeding, infection, fecal incontinence and rarely death.
The Hemwellectomy Procedure: Technique and Mechanism
Hemwellectomy employs a novel electrosurgical unit that delivers a controlled, low-power direct current (<0.1 Watts)16 mA at 6 volts. The procedure is performed with the patient sedated, in the left lateral decubitus position. A two-pronged, round tipped electrode is introduced into the rectum and positioned at the base or directly on the hemorrhoidal tissue. This electrode serves as the cathode, while the anode, a metal plate and saline-soaked sponge (to reduce skin resistance) is placed beneath the patient’s left hip completes the circuit.
Electrophysiological and Biochemical Effects
The non-thermal low-energy direct current initiates several key physiological responses:
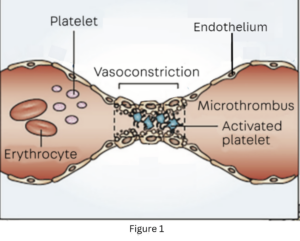
Vasospasm: The current induces rapid sustained contraction of smooth muscle in the terminal branches of the superior rectal artery (arterioles), leading to immediate cessation of blood flow, de-arterializing the hemorrhoid. Fig 1
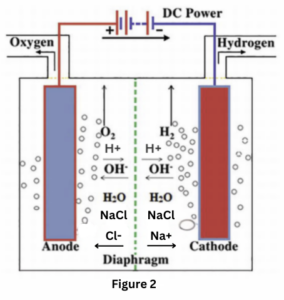
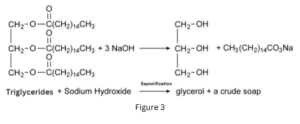
Electrolysis and Saponification: As electrons flow, they cause electrolysis of the electrolyte-rich serum, generating hydrogen gas at the cathode (fig 2) and resulting in the local formation of a basic environment. When the pH exceeds 10, saponification occurs through the reaction of serum triglycerides with sodium hydroxide, forming hydrogen filled soap bubbles that are observed on the hemorrhoid’s surface. (Fig 3)
Platelet Activation and Thrombosis: The combined effect of vasospasm and the electro-biochemical alterations promotes platelet activation and endothelial cell injury, ultimately leading to thrombosis and permanent ligation of the affected arterial branches but not within the hemorrhoid sinuses which if punctured will blead.
Its low power but multifaceted mechanism minimizes collateral tissue damage, thereby preserving the integrity of the overlying rectal mucosa and adjacent tissue explains why Hemwellectomy is relatively painless and safe.
Comparative Efficacy and Safety Profile
Clinical data indicate that Hemwellectomy is highly effective, with complete arterial ligation achieved in over 90% of cases following a single treatment under optimal conditions. Reported adverse effects are minimal—post-procedure discomfort is typically mild and transient, resolving within hours, and pain is observed in less than 1% of patients. In contrast, traditional modalities such as rubber band ligation and surgical hemorrhoidectomy are associated with higher rates of pain and complications. Notably, Hemwellectomy is the sole FDA-approved treatment for all grades of hemorrhoidal disease, providing a significant advantage over existing office-based procedures and surgical techniques.
Conclusion
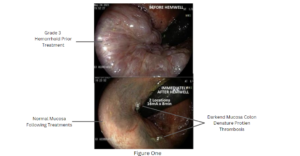
Hemwellectomy offers a paradigm shift in the treatment of hemorrhoidal disease by integrating a non-thermal, low-energy electrosurgical technology with a precise, minimally invasive approach. Its unique mechanism—characterized by targeted vasospasm, controlled electro-biochemical reactions effecting thrombosis—results in rapid hemorrhoidal dearterialization by ligating the afferent circulation and immediate regression of hemorrhoidal tissue to the submucosa with minimal morbidity. (image picture 1) Given its superior safety profile and high clinical efficacy, Hemwellectomy stands as the procedure of choice over older therapies for the broad spectrum of hemorrhoidal disease.
References
- Everhart, J.E. “Burden of Digestive Diseases in the United States Part I: Overall and Upper Gastrointestinal Diseases.” Gastroenterology 2009; 136(2): 376-386.
- Sun, Z. “Review of Hemorrhoid Disease: Presentation and Management.” Clin Colon Rectal Surg. 2016; 29(1): 22–29.
- Aigner, F. “Revised Morphology and Hemodynamics of the Anorectal Vascular Plexus.” Int J Colorectal Dis. 2009; 24(1): 105-113.
- Chung, Y.C. “Endoglin (CD105) Expression in the Development of Hemorrhoids.” 2004; 34: 107-112.
- Andreia, A. “World of GI Surgery.” 2016; 8(9): 614-620.
- Ayman, M. “Rubber Band Ligation for Symptomatic Hemorrhoids.” World J Gastroenterol. 2008; 14(42): 6525–6530.
- Ann R. Coll, A. “Audit of Early Pain Following Band Ligation.” Surg Engl. 2006; 88(3): 275-279.
- Romaguera, V.P. “Postoperative Complications in Hemorrhoidal Disease.” Clin Trials. 2021; 16(1): 67-74.
- Crinton, J., & Abacarian, H. “Benign Anorectal Hemorrhoids.” ASCRS of Colon and Rectal Surgery. 2007.
- Gurevich, V.S. “Platelet Activation in Coronary Artery Spasm.” Blood Coagul Fibrinolysis. 1996; 7(2): 181-182.
- Elaissa, H. “Effect of Locally Applied Electricity on Clot Formation.” Blood Coag Fibrinolysis Factors. 2012.
- Chen, W. “Electroconformational Denaturation of Membrane Proteins.” Ann NY Acad Sci. 2005; 1066: 92-105.
- Andrew, L. “Physiology and Hemostasis.” NCBI, 2023.
- Norman, D. “Direct Current Electrotherapy of Internal Hemorrhoids.” Am J Gastroenterol. 1988.
- Inoue, T. “Detection of Activated Platelets during Hemorrhoidal Dearterialization.” Thromb Haemost. 1998; 79: 1004-1007.
- Olatoke, S. et al. “Direct Current Electrotherapy for Internal Hemorrhoids.” Pan Afr Med J. 2014; 18: 145.
